Case study by Julia and Martin
Dual Immediate Load
Patient assesment
60 year old male presents with serve perio and mobile teeth. This has led to a few teeth over erupting and causing an anterior open bite, also tooth loss over the years. A full assessment is carried out to establish the health of remaining teeth and to plan the best course of action going forward.

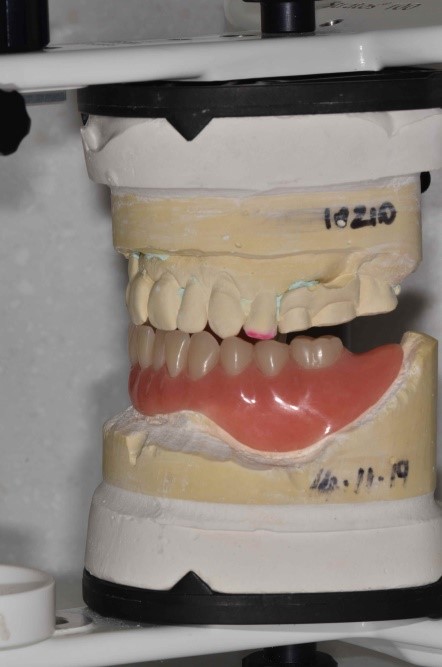
Primary impressions are taken of upper and lower arches and initial bite registration is taken. Models are mounted on an articulator to carry out further assessment.


Restoration and Placement Planning
When it comes to planning these complex cases we always ensure that all elements of the treatment are discussed by all parties involved. The restoring dentist raised some concerns about how we were going to be able to close the anterior open bite when the upper anterior teeth are remaining. I told him the best way to see this was to allow me to do a mock-up of the future tooth position to show him what we could achieve.
I met with the patient for a consultation to discuss the situation and to explain what obstacles we were working against. The patient was happy to go with a more natural set up as this would probably be the best way to achieve a good bite relationship.
Myself and the surgeon on this case looked closely at the CT scan to assess how much bone could be removed to allow for appropriate tooth and implant positioning. After I had gathered all the relevant information I needed I then began to adjust the models. The upper model had to be cut back as the previous partial denture that had been made would not have worked for the new tooth relationship we were aiming for. This then gave me the opportunity to reduce the OVD by 6mm on the articulator so I could close the anterior open bite. A challenging part to this case was that the patient is skeletally class III, so by closing the OVD by 6mm we could increase the prominence of the class III situation. By manipulating the teeth and giving the patient a natural set up I was able to get them in an edge to edge bite relationship and more desirable occlusal plane. The main aim was to give the patient something that was cleansable, functional and aesthetically pleasing.
The surgeon and I met with the patient again to take him through the visual set up and to ensure he was happy with what we had managed to produce. On meeting the patient again the surgeon and I agreed it was a shame that the upper right quadrant was not being immediately loading at the same time as the lower hybrid. At this point we had only immediately loaded either single anterior teeth or full arches but never at the same time. We decided that this was a perfect opportunity and case to see if this was possible.
DAY OF SURGERY
I had made a surgical guide which was an exact clear copy of the set up. This was to enable the surgeon to see the prosthetic envelope we had proposed. All remaining lower teeth were extracted and bone was reduced before the implants were placed.
Once surgery had been successfully carried out, myself and the restoring dentist then set out to pick up the implant componentry in the denture that I had made. This would then be converted into a temporary hybrid bridge.
Unfortunately due to the nature of the case the crown and bridge department had no opportunity to construct or design anything for 024
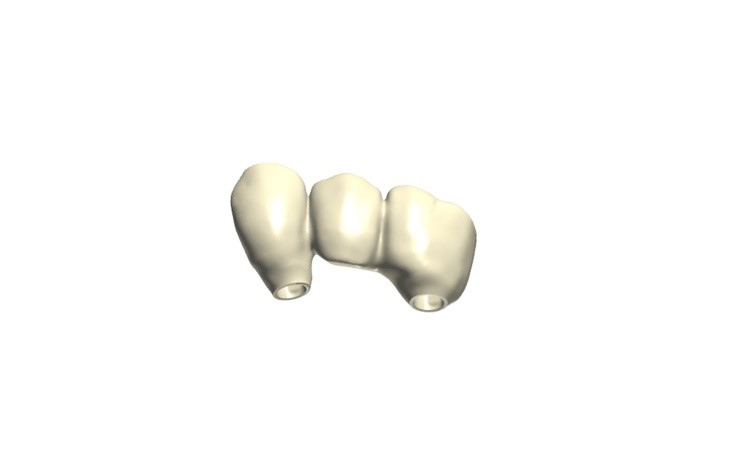
the upper right temporary bridge prior to surgery, which meant all the designing and production had to be carried out on the day. We got the lower denture in place and then scanned the upper right implants and bite registration ready for the upper bridge to be designed.


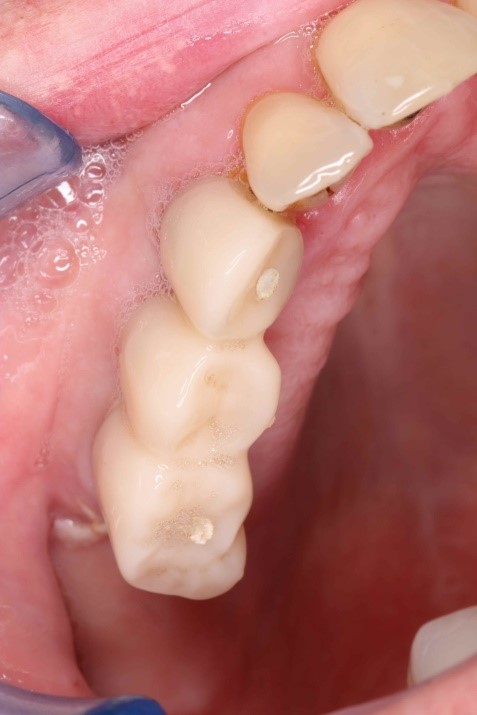
The implants for the upper temporary restoration were placed in the upper right canine and molar site for a temporary 3 unit bridge to be fabricated from PMMA and then fitted on the day of placement opposing the new lower temporary hybrid bridge.
The sulcus formers were scanned along with the scan flags so that the design of the emergence of the bridge would replicate their chamfered design to aid the healing of the surrounding tissues.
The occlusion that had been set by the newly placed lower hybrid bridge was then scanned. With the lower bridge already in place and scanned in occlusion it made fabricating the upper bridge relatively less challenging. The two implants placed for the upper bridge were placed parallel and so we were able to keep the temporary restoration screw retained. The design of the bridge was kept 1mm out of occlusion in order to protect the newly placed implants. Having a preparation scan of the sulcus formers was useful for us as this gives guidance to the emergence of the bridge. With this information it means that we cannot be tempted to over-push the healing tissues or similarly be too passive and cause any tissue resorption. In this situation we are ideally looking to support the tissue whilst developing a good emergence profile.
Due to the nature of the temporary material we always keep a minimum thickness of 1mm to ensure good strength during the healing process.
Finally, the bridge is then bonded to the prepared non-engaging titanium bases in the laboratory.
Conclusion
The outcome of this case was better than we anticipated. The lower temporary hybrid bridge worked and was positioned exactly where we planned it to be. All objectives were met and we managed to fully close the anterior open bite. Being able to provide the patient with an immediately loaded temporary PMMA upper bridge really helped to make this case more aesthetically pleasing for the patient. All parties were delighted with the outcome.
Technicians: Julia Glancey & Martin Bubez
Let's work together



